Did you know healthy adult kidneys can clear about one liter of water per hour? That little fact changes how I think about my water habits.
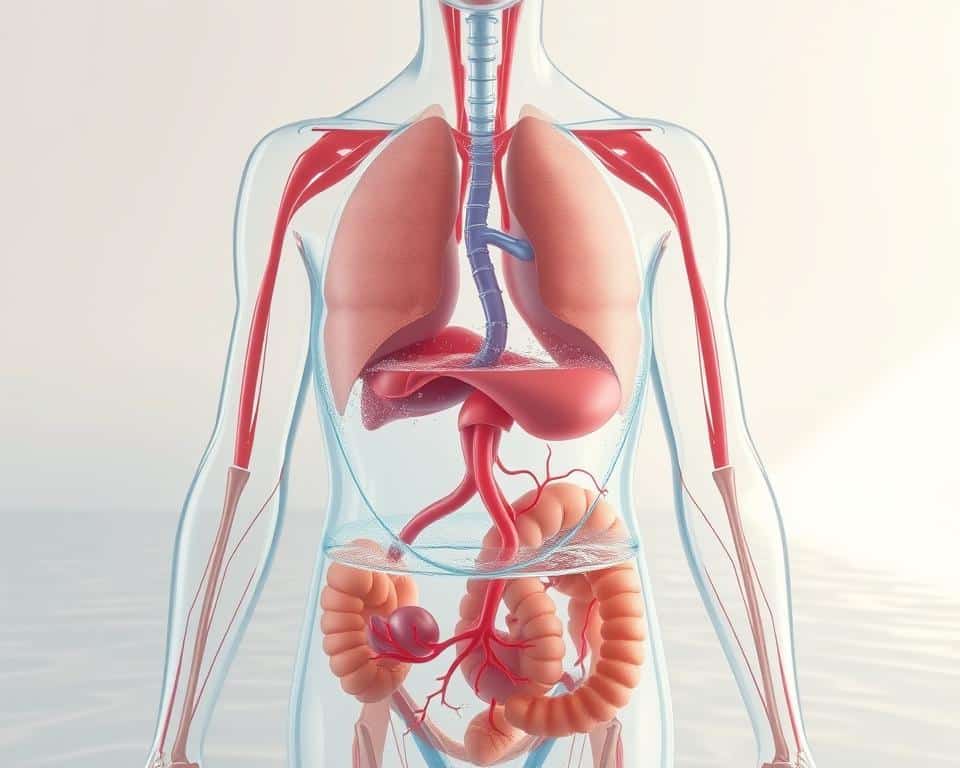
I rely on water to regulate my temperature, move waste, and keep every system working. Drinking too little or too much can both hurt my body and my health.
I explain what water toxicity is in plain terms: when intake or retention outpaces kidney excretion, electrolytes like sodium dilute and cells can swell. Severe drops in sodium may lead to brain swelling, confusion, seizures, or worse.
My quick checks are simple: aim for pale yellow urine, avoid constantly clear urine, and fix dark, tea-colored urine. I follow Institute of Medicine targets as a baseline — about 78–100 ounces for most adults — but I tweak that for heat, workouts, and illness.
This guide gives me clear self-checks, risk factors, and practical steps I actually use to keep water levels balanced and protect my cells and overall condition.
Key Takeaways
- Healthy kidneys typically excrete ~1 liter of water per hour; balance intake to match.
- Aim for pale yellow urine as a simple at-a-glance check.
- Too much water can cause water toxicity and dangerous sodium dilution.
- Daily fluid needs vary; use 78–100 ounces as a starting point and adjust for activity or heat.
- I track simple symptoms and urine color to avoid extremes and protect my health.
How I quickly tell the difference between being overhydrated and dehydrated
I use three fast checks that fit into a busy day. They help me decide whether to sip, hold, or add electrolytes. These cues are easy to repeat and work well during normal activity.
My rapid checks: thirst, energy, and bathroom frequency
I start with thirst. If my mouth is dry and I feel thirsty, I take a small sip and reassess. Thirst usually guides me unless I’m doing long endurance exercise.
I watch energy and head feel. Sluggishness, a dull headache, and low energy point toward needing more fluid. A pressure‑type headache with very clear urine makes me pause.
I track bathroom trips. Healthy people pee about 6–8 times per day; up to 10 can be normal with heavy fluid or caffeine. Much more than usual plus clear urine tells me I may be overdoing it.
Urine color guide and context clues
My color scale is simple: dark tea or apple‑juice color means drink water; lemonade‑pale is my target; clear for hours nudges me to slow down.
I also scan context — hot weather, a long run, or heavy sweat means I need fluids and some electrolytes. I think about the amount I drank recently and whether I gulped many bottles without sodium.
Signs of overhydration vs dehydration
Small clues—headache, urine shade, and stomach queasiness—guide my next move with fluids.
I note clear clusters rather than one single cue. When I feel nausea, vomiting, a throbbing headache, confusion, drowsiness, or muscle cramps after heavy drinking, I consider possible overhydration and water toxicity. In severe cases, seizures, coma, or worse can occur.
What dehydration usually looks like
Thirst, dark or strong‑smelling urine, dizziness, fatigue, dry mouth, and peeing less are the most common clues I see with low fluid. These symptoms push me to sip water and add electrolytes if I’ve been sweating.
How low sodium and the brain interact
Hyponatremia happens when sodium drops below about 135 mEq/L, often from diluting blood with too much plain water.
Low sodium makes brain cells swell, raises intracranial pressure, and can drive confusion, seizures, and coma. I treat sudden confusion or worsening headache as urgent.
When signals overlap and how I reduce guesswork
- I recheck urine color and smell, and think about my intake and sweat in the last 2–4 hours.
- Muscle cramps after lots of sweat plus only water suggest low sodium rather than just low fluid.
- If I feel drowsy or disoriented after rapid drinking, I pause fluids and reassess; worsening mental status prompts medical care.
| Feature | Typical with excess water | Typical with low fluid | What I do |
|---|---|---|---|
| Urine | Very clear, odorless for hours | Dark, strong odor | Compare recent intake and adjust fluids or add electrolytes |
| Head or brain | Throbbing headache, confusion, drowsiness | Dizziness, lightheadedness on standing | Pause drinking if confused; sip with salt if dizzy from heat |
| Muscle | Cramps after lots of plain water and sweat | Cramps with low overall intake | Add sodium if cramps follow heavy sweating |
| Risk | Water toxicity, low sodium levels, brain cell swelling | Reduced blood volume, kidney stress, fatigue | Monitor cluster; seek care for seizures or severe confusion |
Why overhydration happens: drinking too much water or retaining fluid
Rapid drinking and medical factors both raise my risk for dangerous water imbalance. I watch how fast I sip and what else might make my body hold fluid.
Drinking much water too fast: water toxicity and diluted electrolytes
When I drink much water very quickly, my blood sodium can drop. Healthy kidneys clear about one liter per hour, so gulping past that can dilute electrolytes and cause water toxicity.
Health conditions that also make me retain water
Certain disease states can make me retain water even without high intake. Kidney disease, heart failure, cirrhosis, and SIADH can all cause extra fluid to stick around.
Uncontrolled diabetes, low thyroid, or adrenal problems can also change how I handle salt and water. With those conditions, I get specific guidance from my clinician.
Medications and drugs that raise my risk
Some medicines increase thirst or retention. Diuretics, SSRIs/SNRIs, NSAIDs, and MDMA can each raise the chance I’ll retain fluid or crave more water.
- I avoid chugging several bottles quickly because my kidney can only process about a liter an hour.
- I remember that drinking much water too fast can dilute sodium and trigger water toxicity.
- I check my health history and meds; kidney disease, heart failure, liver disease, or SIADH make me cautious about rapid fluid loading.
- During long efforts I use planned electrolytes so I don’t replace sweat losses with only plain water.
How much water I actually need each day
I set a practical daily fluid baseline that I tweak for heat, workouts, and how I feel.
For most healthy adults I use the Institute of Medicine range as my starting point: about 78–100 ounces per day. That amount covers plain drinks and the water in food, like fruit, vegetables, and soup, so I don’t overcount just what I pour.

Daily fluid targets: a flexible baseline
My plan is simple. I aim for the 78–100 ounces range, then add or subtract based on sex, heat, altitude, and activity. On cool, low‑activity days I mostly drink to thirst and watch that my urine stays pale yellow.
Exercise and hot weather: timing and electrolytes
Before workouts I take about 14–22 ounces two to three hours ahead, then sip as needed. For efforts longer than an hour I include sports drinks with sodium and potassium so I replace sweat losses rather than just diluting blood sodium.
- I avoid gulping more than about one liter per hour; pacing helps prevent dilution.
- I track ounces with a marked bottle so my planned amount matches actual intake.
- If I notice consistently clear urine, I modestly cut back until color returns to pale yellow.
My hydration monitoring routine: practical cues and simple metrics
I rely on quick checks and one weighing trick to match what I drink to what I lose. These habits help me keep steady levels and avoid swings that stress my cells.
Urine color and frequency
I check urine each morning. Pale yellow is my goal; dark means I need more water and crystal‑clear for hours makes me pause drinking.
I also log trips to the bathroom. A sudden jump in frequency plus very clear urine tells me to slow intake and reassess recent fluids.
Pre‑ and post‑exercise weigh‑ins
Before and after exercise I weigh myself to estimate sweat loss. One pound lost equals about 16 ounces to replace gradually.
I replace most losses slowly, then top off with meals and normal drinking. For sessions over an hour I add sodium or a sports mix to lower hyponatremia risk.
- I do a quick morning check: pale yellow, not dark or crystal clear.
- I track bathroom frequency and slow down if trips spike with clear urine.
- I weigh pre/post workouts and use the pounds→ounces rule to guide replacement.
- If ankles puff or rings tighten I consider whether I retain water and tweak salt and intake.
| Metric | What I watch | Action |
|---|---|---|
| Urine | Pale yellow vs clear or dark | Adjust water and electrolytes |
| Weight | Pre/post change | Replace ~16 ounces per pound lost gradually |
| Sweat | Duration & intensity during exercise | Use sports drinks for long efforts |
Step‑by‑step: what I do if I suspect overhydration or dehydration
When I think my fluid balance is off, I follow a calm, step‑by‑step plan. I reassess intake, how I feel, and recent activity before changing course.

If I might be overhydrated
I pause any extra drinking for 20–30 minutes. I watch my headache and mental clarity because water toxicity and low sodium can cloud the brain and cause confusion.
If I’ve been sweating a lot, I take a small electrolyte dose with some sodium rather than more plain water. I avoid large fluid boluses and only resume slowly when pressure and clarity improve.
If I might be dehydrated
I sip fluids steadily and check urine color. My goal is pale yellow, not clear or very dark.
After an hour of heavy sweat, I add sodium and potassium with a sports mix to restore sodium levels and aid recovery.
Red flags — when I call for help
I treat severe confusion, seizures, persistent vomiting, trouble breathing, or chest pain as emergencies and go to urgent care or the ER.
If symptoms are unusual or I have chronic illness, I call my primary care for advice before making big fluid changes.
| Situation | Immediate action | When to escalate | Notes |
|---|---|---|---|
| Clear urine + headache | Stop extra drinking, wait 20–30 min | Worsening confusion or seizure | Possible water toxicity; consider small sodium dose if sweaty |
| Dark urine + dizziness | Sip water and oral electrolytes slowly | Persistent vomiting or fainting | Replace gradually; sports drink after >1 hour sweat |
| Rapid intake + lethargy | Hold fluids, monitor mental status | Severe hyponatremia signs | Treatment may include fluid restriction and sodium replacement |
| Chronic disease concern | Call primary care for tailored guidance | New severe or recurring symptoms | Individualized plan based on kidney, heart, liver issues |
For practical daily pacing and bottle counts, I also check resources like how many bottles a day to match intake to activity and avoid flip‑flopping between extremes.
Who’s at higher risk and how I adapt
I pay extra attention when long exercise or health conditions could alter fluid and sodium needs. A few groups need a clear plan so water helps the body, not harms it.
Endurance and long efforts
For marathons, triathlons, long rides, or hikes I pair thirst with a simple plan for fluid and sodium. I estimate sweat rate in training and use that to guide race‑day sips.
I avoid topping off at every aid station and practice my schedule in training. I carry small electrolyte options for heat, altitude, or extra sweat so my cells keep working.
Chronic conditions and tailored limits
If I have kidney disease, heart failure, or liver disease I follow specific volume and sodium limits from my clinician. Certain endocrine issues — SIADH, adrenal problems, or low thyroid — and uncontrolled diabetes can also change how my body handles plain water and salt.
Before big events I check with primary care or a specialist, especially when meds can affect fluid balance.
- I build brief self‑checks during long efforts: urine color on stops, mental clarity, and whether fingers feel puffy.
- I carry electrolyte options and practice my plan in training to avoid last‑minute changes.
| Group | Higher risk why | How I adapt |
|---|---|---|
| Endurance athletes | High sweat losses and long fluid access | Estimate sweat rate, planned sips, use electrolytes |
| Kidney or liver disease | Impaired fluid clearance or retention | Follow individualized volume and sodium limits from clinician |
| Heart failure | Fluid retention and altered salt handling | Coordinate with specialist; monitor weight and swelling |
| Endocrine disorders | SIADH, adrenal or thyroid issues change water handling | Seek tailored guidance and avoid rapid large intakes |
For practical guidance and limits I also review trusted resources like what is too much water intake when I need a refresher before an event or medical visit.
Conclusion
I wrap up by keeping one clear rule: pace how much water I drink and listen to simple cues.
I aim for pale‑yellow urine, avoid constant clear urine, and use the IOM range (about 78–100 ounces) as my starting water need each day. I remember that kidneys clear roughly one liter per hour, so I spread sips rather than gulping much water fast.
I plan electrolytes during long efforts to protect sodium levels and the brain from hyponatremia or water toxicity. If nausea, worsening headache, or fogginess follows drinking, I pause, reassess, and correct slowly.
People with kidney, heart, or liver disease require tailored limits, so I check with primary care. My daily goal: steady pale urine and a clear head — small habits that keep my body balanced.